Home » News » Epidemiology of HPV-Associated Cancers: Changing Trends and Future Burden
Epidemiology of HPV-Associated Cancers: Changing Trends and Future Burden
Posted by anderc8 on Wednesday, November 1, 2017 in News, TIPs 2017.

Krystle A. Lang Kuhs, PhD, MPH
Written by Krystle A. Lang Kuhs, PhD, MPH
A rapid increase in the incidence of oropharyngeal cancer, a type of head and neck cancer, has been reported in many parts of the developed world. This rise has been attributed to an increase in the subset of OPCs caused by oral human papillomavirus (HPV) infection. HPV, a DNA virus, preferentially infects the lymphoid tissues of the oropharynx, including the tonsils in the back of throat (palatine) and the tonsils in the base of tongue. The US is considered the focal point of this growing epidemic, where the incidence of HPV-OPC has risen by more than 200 percent over the past several decades. HPV is now responsible for approximately 75 percent of all OPCs diagnosed within the US and primarily affects young (<60 years of age), white males.
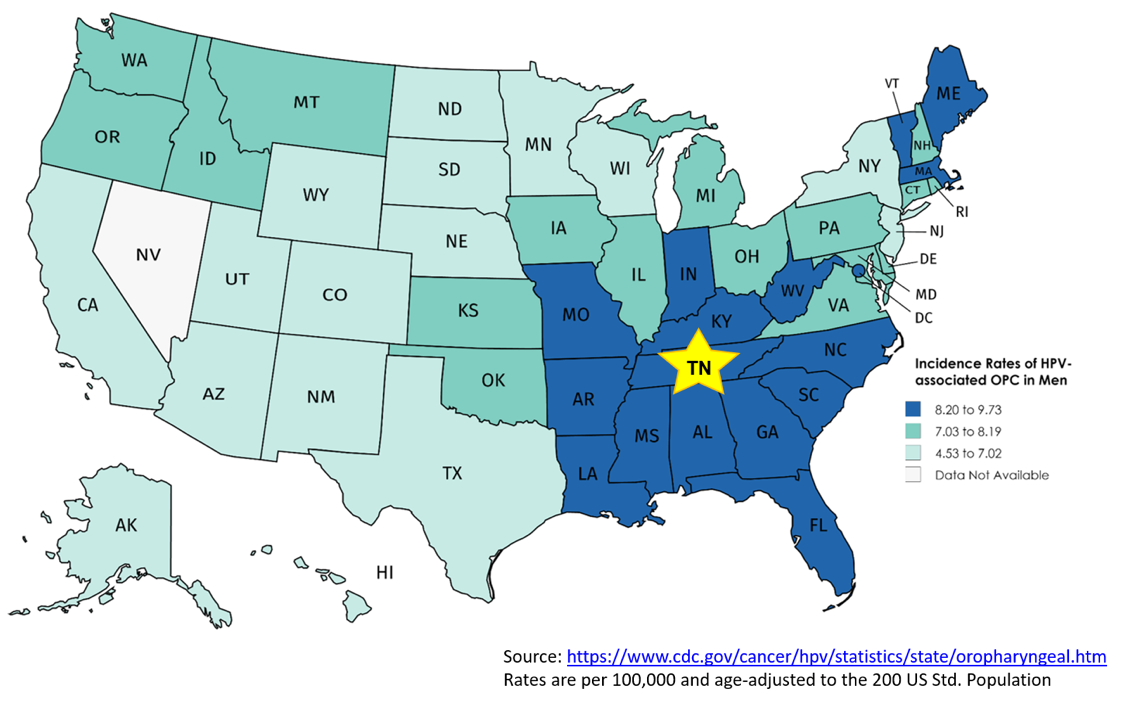
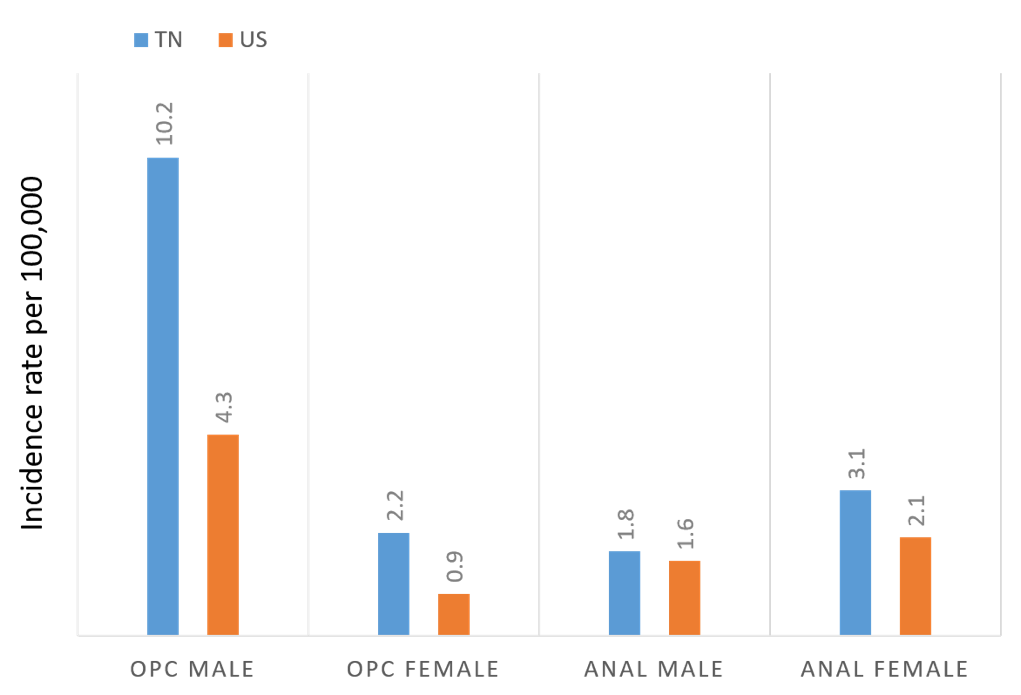
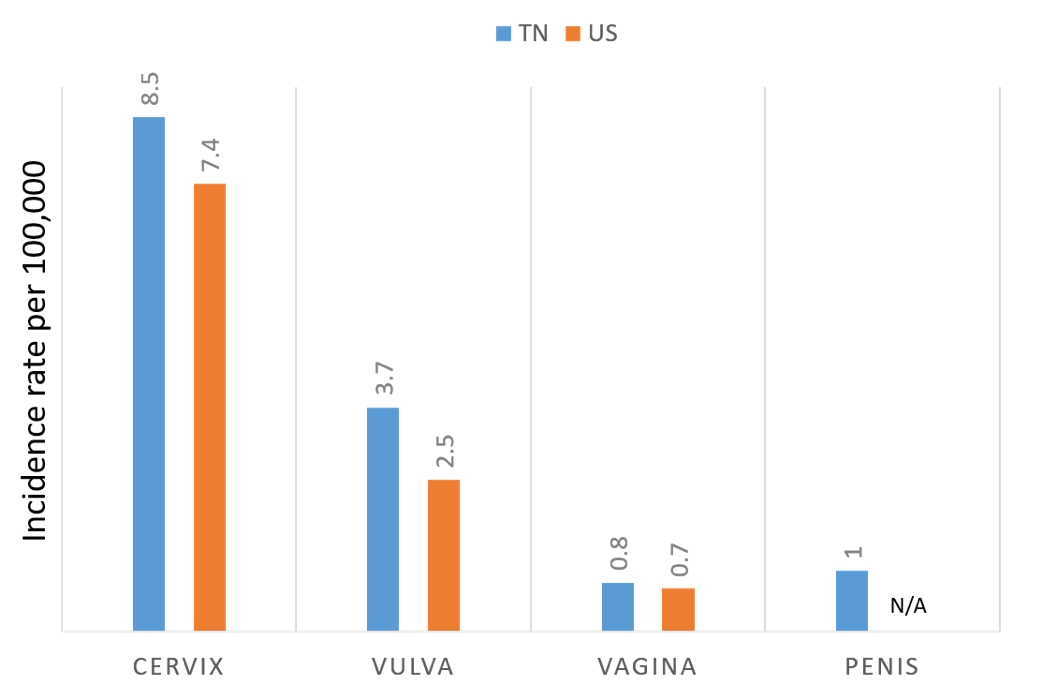
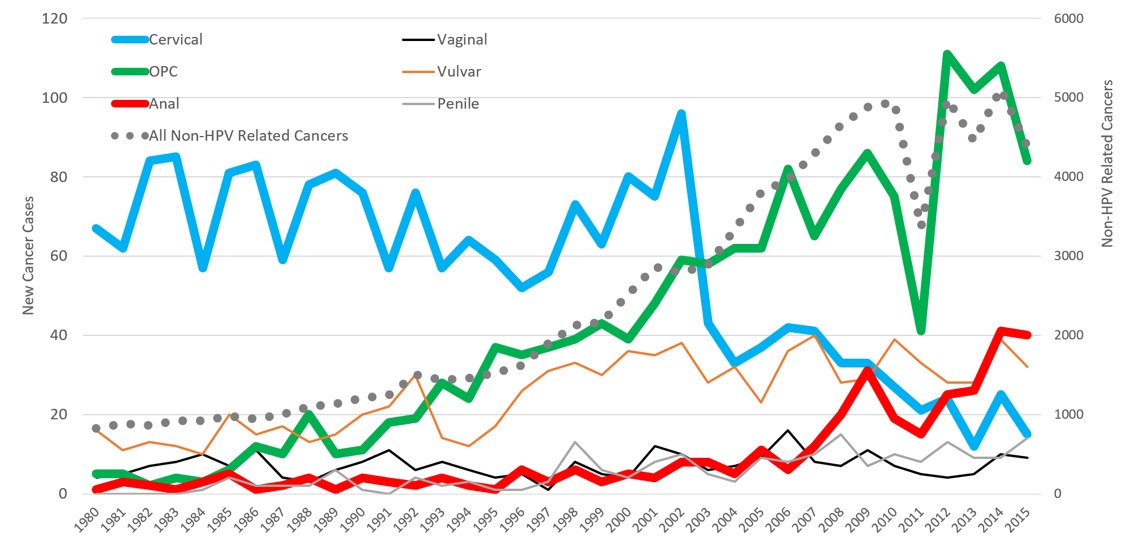
Vanderbilt is at the epicenter of this growing epidemic, as the southeast US has the highest incidence of HPV-associated cancers in the country. In addition to OPC, HPV infection also causes cancers at five other anatomic sites including the cervix, vagina, vulva, penis and anus. In order to combat these HPV-associated cancers, a group of researchers led by Dr. Ronald Alvarez formed the HPV-ACTIVE program, which recently began a study to better understand the burden of HPV-associated cancers in our state and at VUMC. Using Tennessee Department of Health and SEER data, we found that the incidence rate of OPC in Tennessee is more than twice the national average for both males (10.2 vs. 4.3 per 100,000) and females (2.2 vs. 0.9 per 100,000). Compared to national averages, Tennessee also has increased rates of cervical, vulvar and anal cancer in women. The incidence rate of cervical cancer is particularly high among black women at 6.2 per 100,000 compared to 4.2 per 100,000 for white women. Specifically, at our institution, we have seen dramatic increases in the number of both OPC and anal cancer cases diagnosed and/or treated at Vanderbilt over the past few decades. Based on Vanderbilt Cancer Registry data, VUMC diagnoses and/or treats approximately 100 OPC and 40 anal cancers annually.
With the help of a Vanderbilt University Trans-Institutional Programs (TIPs) award, the HPV ACTIVE group is now actively working on the next phase of this study, which will help determine the number and burden of HPV-associated precancers seen at VUMC. Results of this study will be critical for understanding the number of HPV-associated cancer and precancers seen at Vanderbilt to determine the feasibility of conducting specific studies aimed at better preventing these cancers in the future. Areas of active investigation among HPV-ACTIVE members include developing methods to increase HPV vaccine uptake, developing new methods for early detection, and evaluating new diagnostic approaches and treatment options for HPV-associated cancers.
I encourage you to join the conversation. If you have questions or would like to get more involved in the HPV-ACTIVE group, please feel free to contact us or leave a comment below.