Projects
TOOLS: MATLAB and Python (pandas, scikit-learn)
Effect of Cochlear Implant Positioning on Hearing Outcomes
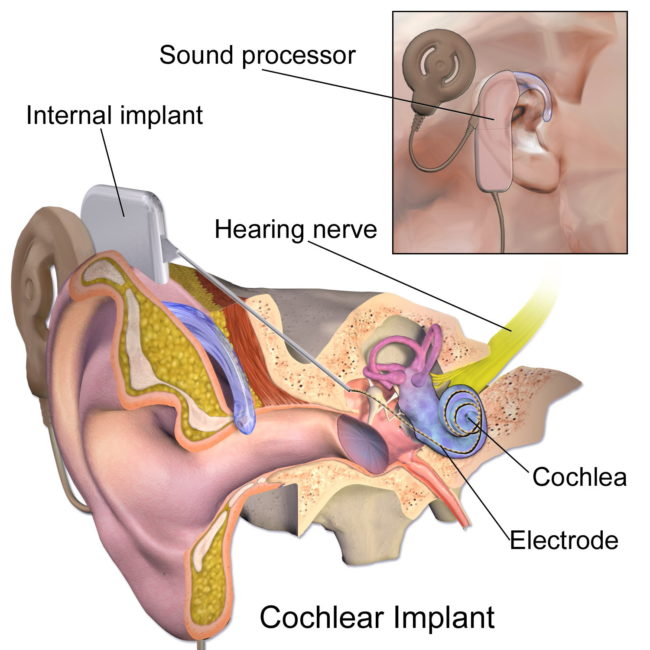
Cochlear Implants are neuroprosthetics that are widely considered the standard of care treatment for patients with at least a moderate sloping to profound sensorineural hearing loss. According to the National Institute on Deafness and Other Communication Disorders (NIDCD), over 324,200 people worldwide have received CIs. The central component of a CI is an electrode array that has to be surgically implanted into the inner ear (figure below) through the round window after temporal mastoidectomy. The activated electrodes stimulate the surviving nerve cells of the spiral ganglia and produce the sensation of sound.
Our aims are
- to identify how positioning affects long term hearing outcomes in adults; and
- how to predict postoperative scores to aid patient-customized preoperative counseling and device choice
Related publication:
- Chakravorti, S.*, Noble, J. H.*, Gifford, R. H., Dawant, B. M., O’Connell, B. P., Wang, J., & Labadie, R. F. (2019). Further Evidence of the Relationship Between Cochlear Implant Electrode Positioning and Hearing Outcomes. Otology & Neurotology, 40(5), 617–624. https://doi.org/10.1097/MAO.0000000000002204
(* indicates co-first authors)
Effects of surgical targeting in LITT for mTLE
Approximately 30 million people worldwide suffer from recurrent disabling seizures due to partial onset epilepsy, which is characterized by seizures arising from a single focal point in the brain. Mesial temporal lobe epilepsy (mTLE) is among the most commonly reported variants of focal epilepsy, accounting for 17-31% of all surgical procedures done for epilepsy. Recently, a minimally invasive alternative to open resection known as laser interstitial thermal therapy (LITT) has gained prominence for epilepsy treatment. Guided by an MRI scanner, surgeons can ablate the epileptogenic focus in the brain with great accuracy using the thermal energy of a laser probe.
Our aims involve
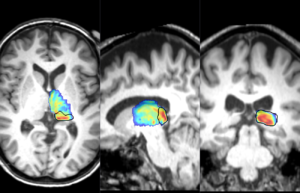
- identify the surgical and demographic factors that affect long term outcomes of seizure freedom
- generate a probability map of optimal surgical targeting locations
Related publications:
- Wu, C.*, Jermakowicz, W. J. *, Chakravorti, S. *, Cajigas, I., Sharan, A. D., Jagid, J.R., . . . D’Haese, P.-F. (2019). Effects of surgical targeting in laser interstitial thermal therapy for mesial temporal lobe epilepsy : A multicenter study of 234 patients. Epilepsia, 60(6), 1171–1183. https://doi.org/10.1111/epi.15565
(* indicates co-first authors) - Chakravorti, S., Jermakowicz, W.J., Wu, C., Li, R., Wirz, R., Dawant, B.M., D’Haese, P.-F. (2019). Evaluation of nonrigid registration around the hippocampus for the construction of statistical maps in a multicenter dataset of epilepsy laser ablation patients. Proc. SPIE 10951, Medical Imaging 2019: Image-Guided Procedures, Robotic Interventions, and Modeling, 109511J (8 March 2019); https://doi.org/10.1117/12.2512587
Effects of CT Image Quality on Localization Accuracy
The accuracy of any image processing algorithm is invariably affected by the image quality. We can define CT image quality by four parameters – orientation of the subject in the scanner, Hounsfield Unit (HU) range of reconstruction of the image, image resolution, and radiation dose of the scan.
Our aim is
- to quantify the sensitivity of image processing algorithms to changes in image parameters
- to control quality of images in our dataset
- to make our algorithms more robust
Related publications:
- Chakravorti, S., Bussey, B. J., Zhao, Y., Dawant, B. M., Labadie, R. F., & Noble, J.H. (2017). Cochlear implant phantom for evaluating computed tomography acquisition parameters. Journal of Medical Imaging, 4(04), https://doi.org/10.1111/epi.15565
- Chakravorti, S., Bussey, B. J., Zhao, Y., Dawant, B. M., Labadie, R. F., & Noble, J.H. (2017). A cochlear implant phantom for evaluating CT acquisition parameters. Proc. SPIE 10135, Medical Imaging 2017: Image-Guided Procedures, Robotic Interventions, and Modeling, 101350N (3 March 2017); https://doi.org/10.1117/12.2255742
Segmentation of the Pulvinar in the Thalamus
The pulvinar of the thalamus is a higher-order thalamic nucleus that is responsible for gating information low to the cortical regions of the brain. Segmenting the pulvinar in clinically acquired images is important to support studies exploring its role in brain function.
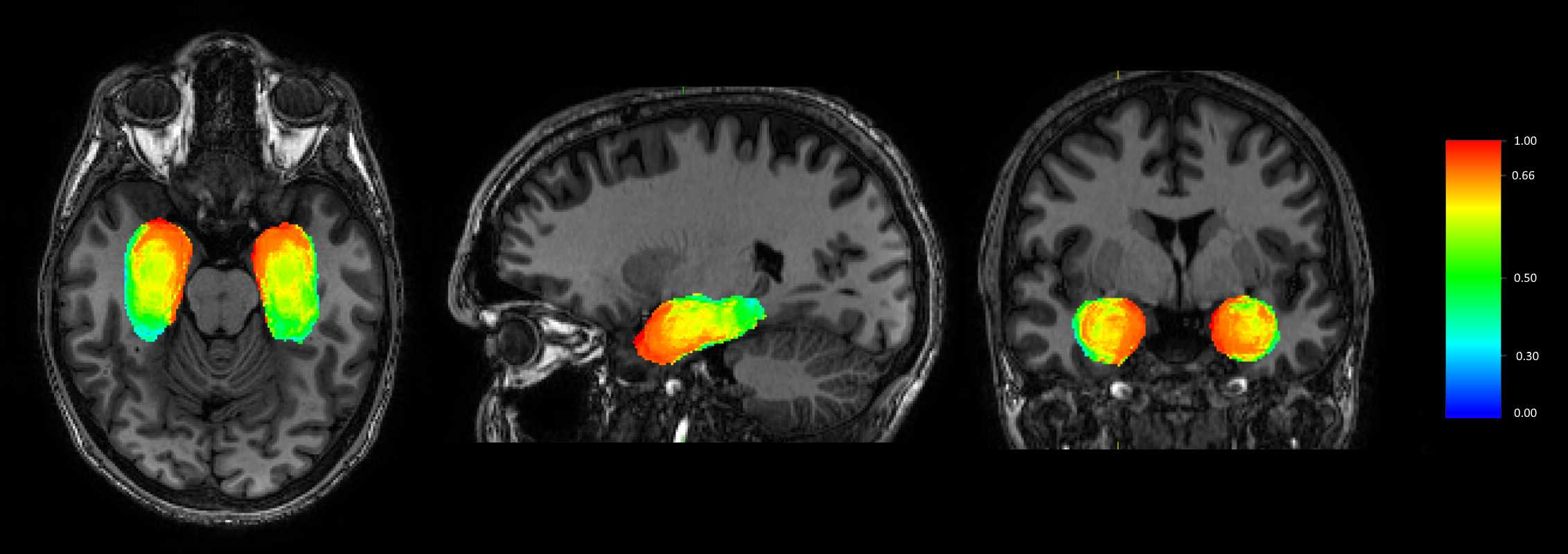
In recent years, we have proposed an active shape model method to segment multiple thalamic nuclei, including the pulvinar. We validate the segmentation of the pulvinar using the known fact that the pulvinar has particularly strong white matter connections to the hippocampus, which allows us to identify the pulvinar from thalamic regions of high hippocampal structural connectivity.
Related publications:
- Chakravorti, S., Morgan, V.L., Trujillo, P., Wirz, R., Dawant, B.M. (2018). A structural connectivity approach to validate a model-based technique for the segmentation of the pulvinar complex. Proc. SPIE 10578, Medical Imaging 2018: Biomedical Applications in Molecular, Structural, and Functional Imaging, 105780T (12 March 2018); https://doi.org/10.1117/12.2293685
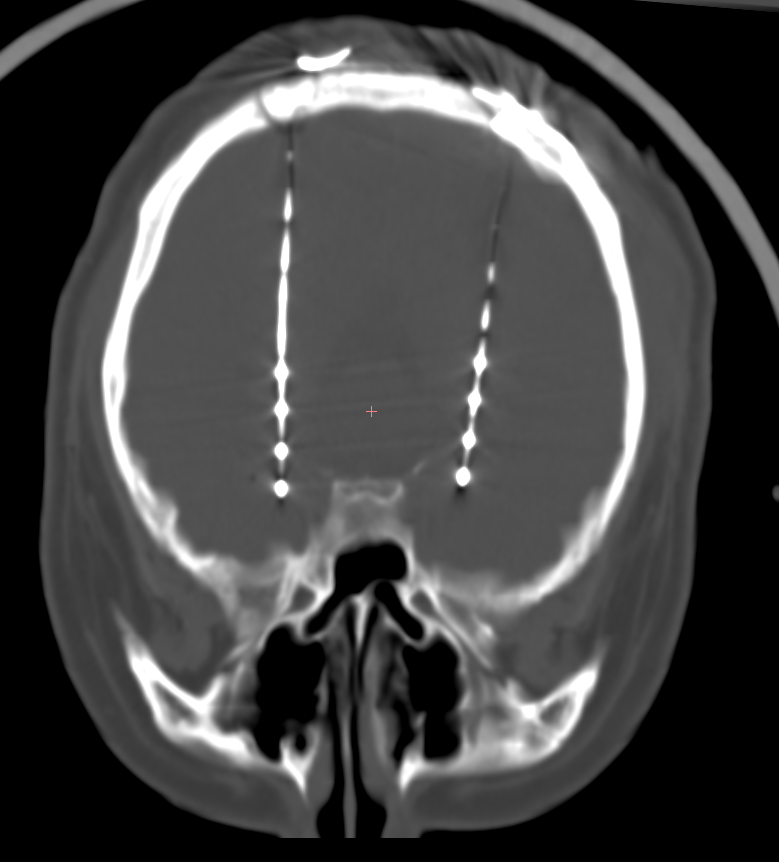
Automatic identification of NeuroPace depth leads in CT images
Responsive neurostimulation (RNS) is a novel surgical intervention for treating medically refractory epilepsy. A neurostimulator implanted under the skull monitors brain activity in one or two seizure foci and provides direct electrical stimulation using implanted electrodes to prevent partial onset seizures. Despite significant successes in reducing seizure frequency over time, outcomes are less than optimal in a number of patients. To maximize treatment efficacy, it is critical to identify the factors that contribute to the variance in outcomes, including accurate knowledge of the final electrode location. However, there is as yet no automated algorithm to localize the RNS electrodes in the brain. Currently, physicians manually demarcate the positions of the leads in postoperative images, a method that is affected by rater bias and is impractical for largescale studies. In this paper, we propose an intensity feature based algorithm that can automatically identify the electrode positions in postoperative CT images. We also validate the performance of our algorithm on a multicenter dataset of 13 implanted patients and test how it compares with expert raters.
Related publications:
- Chakravorti, S., Li, R., Rodriguez, W., Shults, R., Sharan, A., Englot, D.J., Konrad, P.E., D’Haese, P.-F., Dawant, B.M. (2018). Validation of an automatic algorithm to identify NeuroPace depth leads in CT images. Proc. SPIE 10951, Medical Imaging 2019: Image-Guided Procedures, Robotic Interventions, and Modeling, 109512D (8 March 2019); https://doi.org/10.1117/12.2512580