Therapies for Tumor-Induced Bone Disease
Self Assembled Nanoparticles for Drug Delivery

Self assembled nanoparticles can be generated by polymerizing hydrophobic and hydrophilic monomers via RAFT based synthetic routes. The properties of the nanoparticles, such as drug loading, size, and drug release rates, can be adjusted by changing the monomeric components. This project aims to generate synthetic nanoparticle carriers for novel drugs used to combat tumor-induced bone disease. Major collaborators are from the Sterling (Clinical Pharmacology) and Duvall (Biomedical Engineering) groups.
Tissue-Engineered Bone Constructs
 Tumor-induced bone disease is regulated by a complex interaction between tumor cells and the microenvironment. Recently, we published that the rigidity of 2D substrates can influence tumor cell gene expression. We hypothesize that a combination of the rigid bone matrix and the cellular content of the bone marrow are required for tumor cells to induce bone destruction. Studying these interactions in vivo is complicated. Furthermore, the limitations of 2D experiments are well known. Therefore, we have designed 3D tissue-engineered bone constructs (TEBCs) mimicking the bone microenvironment. TEBCs are generated by reactive liquid molding of polymer-ceramic hybrid precursors in a 3D-printed template. The resulting scaffolds stimulate osteoblast differentiation and are resorbed by osteoclasts. Mechanical and topological properties can be tailored to recapitulate the properties of healthy or diseased trabecular bone. We are investigating the progression of tumor-induced bone disease and drug response in patient-derived tumor cells using this technology.
Tumor-induced bone disease is regulated by a complex interaction between tumor cells and the microenvironment. Recently, we published that the rigidity of 2D substrates can influence tumor cell gene expression. We hypothesize that a combination of the rigid bone matrix and the cellular content of the bone marrow are required for tumor cells to induce bone destruction. Studying these interactions in vivo is complicated. Furthermore, the limitations of 2D experiments are well known. Therefore, we have designed 3D tissue-engineered bone constructs (TEBCs) mimicking the bone microenvironment. TEBCs are generated by reactive liquid molding of polymer-ceramic hybrid precursors in a 3D-printed template. The resulting scaffolds stimulate osteoblast differentiation and are resorbed by osteoclasts. Mechanical and topological properties can be tailored to recapitulate the properties of healthy or diseased trabecular bone. We are investigating the progression of tumor-induced bone disease and drug response in patient-derived tumor cells using this technology.
================================
Regeneration of Cutaneous Tissue and Scarless Wound Healing
Cell Delivery
 In order to apply mammalian regenerative cells have shown promise for cell therapy, there is a compelling need for suitable polymeric carriers that can provide a scaffold for adhesion of transplanted cells. Lysine-derived polyurethane scaffolds, which are porous, biodegradable, and biocompatible, have been reported to support cellular infiltration and new tissue formation in subcutaneous, cardiovascular, and bone models. Due to their injectability and ability to cure in situ, two-component lysine-derived polyurethanes are promising carriers for local delivery of cells using minimally invasive surgical techniques.
In order to apply mammalian regenerative cells have shown promise for cell therapy, there is a compelling need for suitable polymeric carriers that can provide a scaffold for adhesion of transplanted cells. Lysine-derived polyurethane scaffolds, which are porous, biodegradable, and biocompatible, have been reported to support cellular infiltration and new tissue formation in subcutaneous, cardiovascular, and bone models. Due to their injectability and ability to cure in situ, two-component lysine-derived polyurethanes are promising carriers for local delivery of cells using minimally invasive surgical techniques.
We used injectable polyurethanes synthesized from a polyester triol, an iron acetylacetonate catalyst, and a lysine triisocyanate-PEG (LTI-PEG) prepolymer, as carriers for cell delivery. Delivered cells were encapsulated in alginate hydrogel to protect cells from the generated harmful reaction products and cells were proved to survive long term both in vitro and in vivo.
Nucleic Acid Delivery
 Nonviral gene therapy has potential for use in tissue regeneration and treatment of diseases, but many of the traditional transfection reagents such as polyethylenimine (PEI) suffer from instability and aggregation, especially when lyophilized for storage and/or incorporation into biomaterial scaffolds. A novel library of diblock copolymers were developed and screened for improved stability and nucleic acid transfection following lyophilization. The studies were motivated by the desire to prepare a plasmid DNA (pDNA) nanocarrier that is stable through lyophilization and fabrication of tissue engineering scaffolds in order to improve bioactivity in vivo. The novel diblock copolymers had smaller sizes after lyophilization, less aggregation in the presence of salt, and higher transfection efficiency than PEI polyplexes. Future work will involve incorporating lyophilized diblock copolymer-pDNA nanoparticles into polyurethane scaffolds for in vivo gene therapy applications.
Nonviral gene therapy has potential for use in tissue regeneration and treatment of diseases, but many of the traditional transfection reagents such as polyethylenimine (PEI) suffer from instability and aggregation, especially when lyophilized for storage and/or incorporation into biomaterial scaffolds. A novel library of diblock copolymers were developed and screened for improved stability and nucleic acid transfection following lyophilization. The studies were motivated by the desire to prepare a plasmid DNA (pDNA) nanocarrier that is stable through lyophilization and fabrication of tissue engineering scaffolds in order to improve bioactivity in vivo. The novel diblock copolymers had smaller sizes after lyophilization, less aggregation in the presence of salt, and higher transfection efficiency than PEI polyplexes. Future work will involve incorporating lyophilized diblock copolymer-pDNA nanoparticles into polyurethane scaffolds for in vivo gene therapy applications.
================================
Injectable and Settable Bone Grafts
Reactivity and Biocompatibility of Injectable Polyurethane Biocomposites
 Injectable and settable bone grafts offer significant advantages over pre-formed implants due to their ability to be administered using minimally invasive techniques and to conform to the shape of the defect. However, injectable biomaterials present biocompatibility challenges due to the potential toxicity and ultimate fate of reactive components that are not incorporated in the final cured product. The effects of stoichiometry and catalyst concentration on the reactivity, injectability, and biocompatibility of two-component lysine-derived polyurethane (PUR) biocomposites were investigated. Rate constants were measured for the reactions of water (a blowing agent resulting in the generation of pores), polyester triol, dipropylene glycol (DPG), and allograft bone particles with the isocyanate-terminated prepolymer using an in situ ATR-FTIR technique. Based on the measured rate constants, a kinetic model predicting the conversion of each component with time was developed. The PUR biocomposite supported cellular infiltration and remodeling in femoral condyle defects in rabbits at 8 weeks, and there was no evidence of an adverse inflammatory response induced by unreacted components from the biocomposite or degradation products from the cured polymer. Taken together, these data underscore the utility of the kinetic model for predicting the biocompatibility of reactive biomaterials.
Injectable and settable bone grafts offer significant advantages over pre-formed implants due to their ability to be administered using minimally invasive techniques and to conform to the shape of the defect. However, injectable biomaterials present biocompatibility challenges due to the potential toxicity and ultimate fate of reactive components that are not incorporated in the final cured product. The effects of stoichiometry and catalyst concentration on the reactivity, injectability, and biocompatibility of two-component lysine-derived polyurethane (PUR) biocomposites were investigated. Rate constants were measured for the reactions of water (a blowing agent resulting in the generation of pores), polyester triol, dipropylene glycol (DPG), and allograft bone particles with the isocyanate-terminated prepolymer using an in situ ATR-FTIR technique. Based on the measured rate constants, a kinetic model predicting the conversion of each component with time was developed. The PUR biocomposite supported cellular infiltration and remodeling in femoral condyle defects in rabbits at 8 weeks, and there was no evidence of an adverse inflammatory response induced by unreacted components from the biocomposite or degradation products from the cured polymer. Taken together, these data underscore the utility of the kinetic model for predicting the biocompatibility of reactive biomaterials.
Injectable, Settable Bone Grafts Augmented with rhBMP-2 for Healing of Craniofacial Bone Defects
 Growth factors incorporated into scaffolds for tissue engineering promote the infiltration of cells and tissue. Recombinant human bone morphogenetic growth factor-2 (rhBMP-2) stimulates osteoblast differentiation and new bone formation when delivered locally. Biodegradable polyurethane (PUR) biocomposites incorporating allograft bone particles have been reported to be effective carriers for rhBMP-2 and support new bone growth. However, allograft presents both biological and regulatory challenges. Delivery of even a low dose of rhBMP-2 combined with allograft can result in transient resorption. Injectable, settable bone grafts with resorbable fillers provide a platform for rhBMP-2 delivery. We are investigating the dose response of rhBMP-2 with a variety of synthetic fillers for bone healing.
Growth factors incorporated into scaffolds for tissue engineering promote the infiltration of cells and tissue. Recombinant human bone morphogenetic growth factor-2 (rhBMP-2) stimulates osteoblast differentiation and new bone formation when delivered locally. Biodegradable polyurethane (PUR) biocomposites incorporating allograft bone particles have been reported to be effective carriers for rhBMP-2 and support new bone growth. However, allograft presents both biological and regulatory challenges. Delivery of even a low dose of rhBMP-2 combined with allograft can result in transient resorption. Injectable, settable bone grafts with resorbable fillers provide a platform for rhBMP-2 delivery. We are investigating the dose response of rhBMP-2 with a variety of synthetic fillers for bone healing.
Settable Bone Grafts for Repair of Weight-Bearing Bone Defects
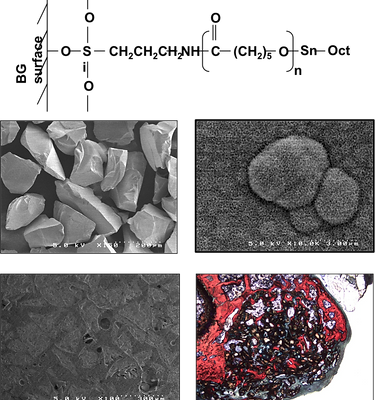 Injectable, settable bone grafts that possess initial mechanical strength exceeding that of host bone and maintain strength comparable to bone while remodeling could improve the clinical management of a number of orthopaedic conditions, such as repair of open tibial plateau fracture, screw augmentation, and vertebroplasty. In tibial plateau fractures, calcium phosphate cements (CPCs) have proven to be superior to autograft, as evidenced by a retrospective study reporting that 61% of patients treated with buttress plating and autograft experienced loss of reduction after one year compared to 23% of patients treated with a hydroxyapatite (HA) bone cement. However, the brittleness and low shear strength of CPCs, as well as their slow remodeling, can result in prolonged recovery times, joint stiffness, and cost to society. Injectable polyurethane (PUR) biocomposites are an attractive alternative to calcium phosphate cements due to their tough mechanical properties and active remodeling. 45S5 bioactive glass (BG) has widely been used for bone regeneration purposes due to its osteoconductivity and bioactivity.
Injectable, settable bone grafts that possess initial mechanical strength exceeding that of host bone and maintain strength comparable to bone while remodeling could improve the clinical management of a number of orthopaedic conditions, such as repair of open tibial plateau fracture, screw augmentation, and vertebroplasty. In tibial plateau fractures, calcium phosphate cements (CPCs) have proven to be superior to autograft, as evidenced by a retrospective study reporting that 61% of patients treated with buttress plating and autograft experienced loss of reduction after one year compared to 23% of patients treated with a hydroxyapatite (HA) bone cement. However, the brittleness and low shear strength of CPCs, as well as their slow remodeling, can result in prolonged recovery times, joint stiffness, and cost to society. Injectable polyurethane (PUR) biocomposites are an attractive alternative to calcium phosphate cements due to their tough mechanical properties and active remodeling. 45S5 bioactive glass (BG) has widely been used for bone regeneration purposes due to its osteoconductivity and bioactivity.
We have investigated the effects of BG surface modification on the bioactivity and mechanical properties of PUR/BG composites. Prior to reaction with the PUR binder, BG particles were functionalized with the silane-coupling agent 3-aminopropyl-trietoxysilane (APTES), which has been shown to increase the mechanical compressive strength of BG, as well as surface grafting of polycaprolactone (PCL) to enhance interfacial bonding.