Home » News » Organs-on-Chips Pave the Way for Endometriosis Research
Organs-on-Chips Pave the Way for Endometriosis Research
Posted by anderc8 on Monday, February 13, 2017 in News, TIPs 2015.
Written by Vanderbilt University Graduate Student Juan Gnecco (Working in Dr. Kevin Osteen’s lab, which is affiliated with the Pre3 Initiative)
In an exciting age of innovation and technological advancements, biomedical researchers are uniquely positioned to integrate interdisciplinary fields in order to better understand some of the most complex and deadly diseases. The Vanderbilt Pre3 Initiative (Preventing adverse Pregnancy outcomes and Prematurity) exemplifies this by merging engineers, educators, clinicians and scientists who share an interest in reducing the burden of reproductive disorders. The Osteen and Bruner-Tran labs, as part of the obstetrics and gynecology (Ob-Gyn) department at Vanderbilt University Medical Center, is highly invested in understanding how exposures to environmental toxicants, such as endocrine disrupting chemicals, may contribute to reproductive tract disorders like preterm birth, infertility and endometriosis.
 The National Institutes of Health National Toxicology Program estimates that more than 80,000 chemicals have been released into our environment over the past few decades and little data exists to assess the potential risk of these toxicants to human populations. Our interests extend from the pre-conception toxicant exposures of the endometrium, the tissue in the inner lining of the uterus that is responsible for establishing pregnancy, to the uterus during the late stages of pregnancy. Using human cells from donors and animal models, we have focused on understanding how the influence of developmental and adult environmental exposures leads to reproductive disease and dysfunction such as endometriosis and premature birth. Endometriosis is a common gynecologic disorder characterized by the presence of endometrial tissue dispersed in extrauterine locations and manifests itself with severe and debilitating pelvic pain. The prevalence of endometriosis is 5-10 percent in all women of reproductive age and 40-60 percent in women with pain and infertility. It represents the single major cause for hysterectomies in reproductive age women with an estimated societal cost of nearly $69.4 billion per year. This disease remains to be one of the most poorly understood conditions affecting women’s reproductive health and has been associated with infertility, abnormal bleeding and spontaneous preterm birth. Preterm birth is as live birth prior to 37 weeks of pregnancy. According to the World Health Organization, every year an estimated 15 million babies are born preterm and complications from these preterm births are the leading cause of death among children under 5 years of age, responsible for nearly 1 million deaths in 2013. Despite its prevalence and socio-economic implications, the cause of endometriosis or preterm birth is still unknown. However, a link between environmental toxicants and the development of these reproductive tract disorders has been identified and may explain why certain subsets of the populations are more susceptible to develop endometriosis, infertility or be prone to undergo preterm labor.
The National Institutes of Health National Toxicology Program estimates that more than 80,000 chemicals have been released into our environment over the past few decades and little data exists to assess the potential risk of these toxicants to human populations. Our interests extend from the pre-conception toxicant exposures of the endometrium, the tissue in the inner lining of the uterus that is responsible for establishing pregnancy, to the uterus during the late stages of pregnancy. Using human cells from donors and animal models, we have focused on understanding how the influence of developmental and adult environmental exposures leads to reproductive disease and dysfunction such as endometriosis and premature birth. Endometriosis is a common gynecologic disorder characterized by the presence of endometrial tissue dispersed in extrauterine locations and manifests itself with severe and debilitating pelvic pain. The prevalence of endometriosis is 5-10 percent in all women of reproductive age and 40-60 percent in women with pain and infertility. It represents the single major cause for hysterectomies in reproductive age women with an estimated societal cost of nearly $69.4 billion per year. This disease remains to be one of the most poorly understood conditions affecting women’s reproductive health and has been associated with infertility, abnormal bleeding and spontaneous preterm birth. Preterm birth is as live birth prior to 37 weeks of pregnancy. According to the World Health Organization, every year an estimated 15 million babies are born preterm and complications from these preterm births are the leading cause of death among children under 5 years of age, responsible for nearly 1 million deaths in 2013. Despite its prevalence and socio-economic implications, the cause of endometriosis or preterm birth is still unknown. However, a link between environmental toxicants and the development of these reproductive tract disorders has been identified and may explain why certain subsets of the populations are more susceptible to develop endometriosis, infertility or be prone to undergo preterm labor.
At the Osteen lab, we strive to understand how exposure to toxicants can disrupt the female reproductive tract and contribute to pregnancy-related complications and diseases. To accomplish this goal, we are integrating innovative biomedical engineering approaches to develop models known as “Organs-on-Chips” (OoCs) of the female reproductive tract. These small-scale models are designed to represent a human organ. These devices house all of the cells that make up an organ into one system in order to understand how they “talk” to each other and maintain the function of the tissue. With the collaboration from engineers, immunologists, toxicologists and researchers from Vanderbilt University, as well as colleagues from the University of Leeds, UK, Massachusetts Institute of Technology (MIT), and the University of Pittsburgh, we are developing OoCs that mimic the context and complexity of human uterine tissue.
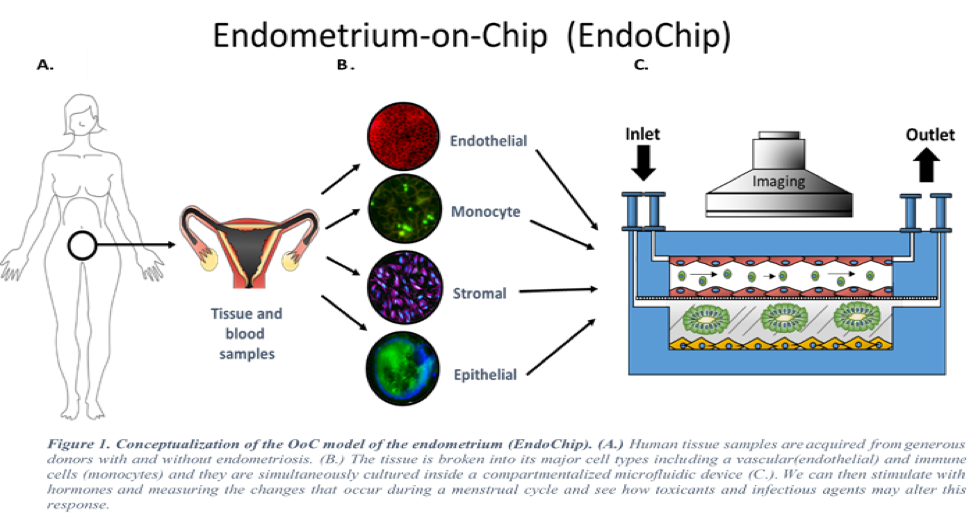
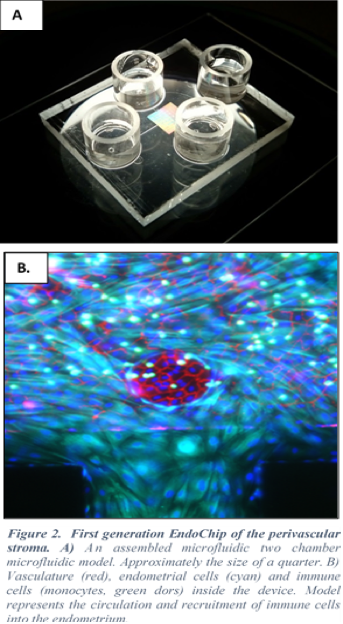
We have recently developed a first generation of the Endometrium-on-Chip (EndoChip) which offers the ability to identify, in detail, the role of the human uterus. We are able to mimic and measure how hormones and immune cells regulate the reproductive function. These models have the ability to maintain and control the cells that make up a uterus for long periods of time (greater than 28 days). Thus, the “EndoChip” allows us to mimic and measure the changes that a uterus undergoes during an idealized human 28-day menstrual cycle. These models can provide insight into how environmental toxicants may alter cells within these tissues and promote dysfunction. These innovative models offer the potential to screen, identify and test new therapeutic approaches for endometriosis.
Much like the “EndoChip”, we are applying this technology to develop an “Instrumented Fetal Membrane on a Chip” (IFMOC), that mimics the fetal membrane for preterm birth research. Together, these models will provide insight into both early and late pregnancy events and how toxicants may promote reproductive disorders. Thus, OoCs are expected to have a major impact on drug discovery, screening, and assessment of efficacy and safety.
We encourage you to learn more about microfluidic Organs-on-Chips by listening to the TedTalk “Body parts on a chip” or by contacting the Osteen or Bruner-Tran labs directly to learn more about endometriosis, preterm birth, reproductive toxicology or Organs-on-Chips (Kevin.Osteen@vanderbilt.edu, kaylon.bruner-tran@vanderbilt.edu or juan.s.gnecco@vanderbilt.edu).
Furthermore, we invite you join the conversation by leaving comments or asking questions in the space provided below.
