Home » News » Leveraging Quality Improvement Efforts to Increase HPV Vaccination Rates in Tennessee
Leveraging Quality Improvement Efforts to Increase HPV Vaccination Rates in Tennessee
Posted by anderc8 on Tuesday, May 29, 2018 in News, TIPs 2017.
Written by Pamela C. Hull, Ph.D., and Kelsey Minix, MPH Student
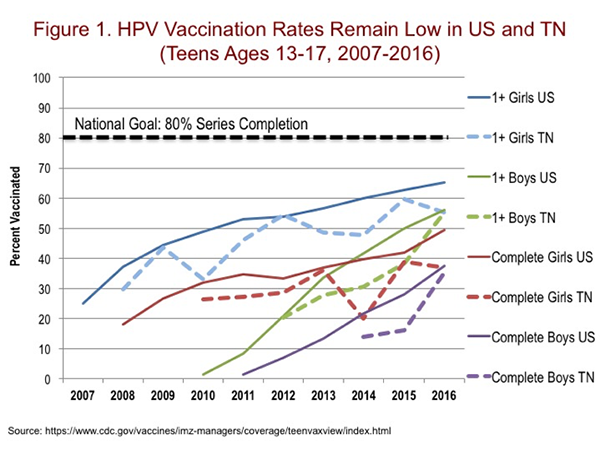
HPV (human papillomavirus) vaccination is an important component to adolescent health because it protects against six cancers (cervical, oropharyngeal, anal, penile, vaginal and vulvar) and genital warts caused by the HPV infection. Despite the benefits of cancer prevention, HPV vaccination rates in the US and Tennessee remain relatively low (see Figure 1). A greater burden of HPV-associated cancers in Tennessee and the Southeast compared to the US overall point to the need for local efforts to increase HPV vaccination coverage. With healthcare provider recommendations being the strongest predictor of HPV vaccine uptake, a top priority is improving the quality of care relative to HPV vaccination in the primary care setting.
Dr. Hull and her colleagues are conducting a study funded by the HPV ACTIVE TIPs award, in collaboration with the Cumberland Pediatric Foundation (CPF). The goal is to test a model for disseminating a web-based quality improvement coaching program to pediatric clinics. The team has been adapting a web portal that will help clinics and physicians implement quality improvement projects focused on increasing immunization rates. As an incentive to participate, physicians will receive Maintenance of Certification (MOC) Part IV credits to help fulfill their MOC requirements under the American Board of Pediatrics. The main focus in adapting the web portal is to automate the process as much as possible for clinics and the managing staff at Vanderbilt and CPF so it can be delivered on a large scale at a low cost. This summer, the team will finalize the web portal automation and start pilot testing to make any additional needed refinements. After the pilot testing phase, the team will start signing up clinics to use the web portal for MOC quality improvement projects and guide them on how to track their HPV vaccination rates over time. The team will also collect surveys of the physicians and administrative staff to assess motivations, acceptability, obstacles and costs for implementing the program. This pilot will inform the development of a future grant proposal to study the processes of disseminating the web portal intervention on a larger scale across the Tennessee and beyond.
We have also been examining existing data sources to identify disparities in HPV vaccination rates. Kelsey Minix, a Masters of Public Health (MPH) student funded by the HPV ACTIVE project, conducted an analysis of the relationship between urbanicity and HPV vaccination. It is likely that one’s regional location can influence culture, access to resources and knowledge of the HPV vaccination. Using National Immunization Survey-Teen (NIS-Teen) data, we compared HPV vaccine initiation and completion rates among populations in urban, suburban and rural areas in the 50 states. Our results showed that within certain states, HPV vaccine completion and initiation rates are higher in urban areas versus suburban and rural areas (Figure 2). This implies that in the future, when we are determining how to improve HPV vaccination uptake, we need to consider geographical area and how that influences patients’ HPV vaccination decisions.
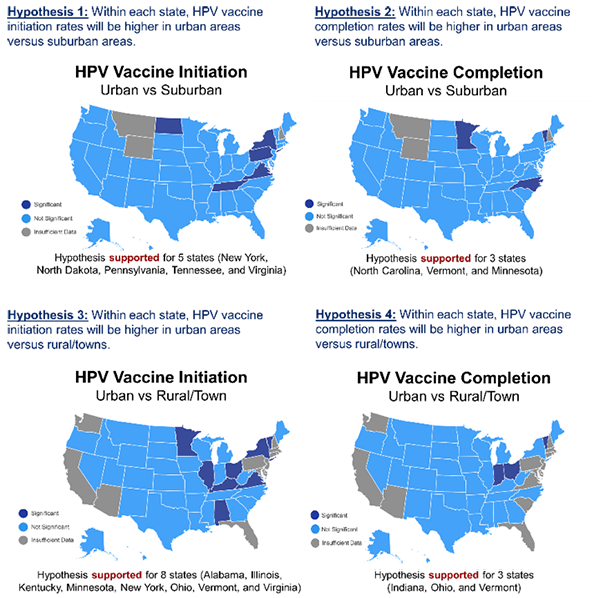
State-Level Geographic Comparisons of HPV Initiation and Completion Rates
