Home » News » Human Milk as a Source of Narrow Spectrum Antimicrobial Agents
Human Milk as a Source of Narrow Spectrum Antimicrobial Agents
Posted by anderc8 on Monday, January 29, 2018 in News, TIPs 2015.

Assistant Professor of Chemistry Steven Townsend
Written by Steven Townsend, Assistant Professor of Chemistry
Antimicrobial resistance is among the most complex and alarming public health challenges facing society. Warnings that antibiotics are losing their effectiveness due to misuse and overuse have been largely ignored by clinicians and the public, and the world’s most widespread infectious diseases (HIV, malaria and tuberculosis) are becoming more difficult to treat due to drug resistance. Infections caused specifically by antibiotic-resistant bacteria continue to challenge the clinic. The World Health Organization (WHO) has shown that rates of infection attributable to methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus faecium (VRE) and fluoroquinolone-resistant Pseudomonas aeruginosa are rapidly increasing. In fact, more patients in the United States die each year from MRSA than from HIV, AIDS and tuberculosis combined.
Historically, big pharma has been the largest source of therapeutics in the world. Perhaps paradoxically, however, these companies have minimal investment in the development of new antibiotics as the financial return is very low. In the Townsend lab, we have interest in developing novel strategies to treat infectious diseases, specifically in the context of bacterial pathogens. Recently, our attention turned to human milk, the gold standard for infant wellness. Breastfed infants experience decreased instances of diarrhea, respiratory infection, urinary tract infection, ear infection, necrotizing enterocolitis (NEC) and sudden infant death syndrome (SIDS), compared to their formula-fed counterparts. Based on the volume of studies detailing the ability of human milk oligosaccharides (HMOs) to provide these benefits, we hypothesized these molecules could also function as antimicrobial and antibiofilm agents against bacterial pathogens.
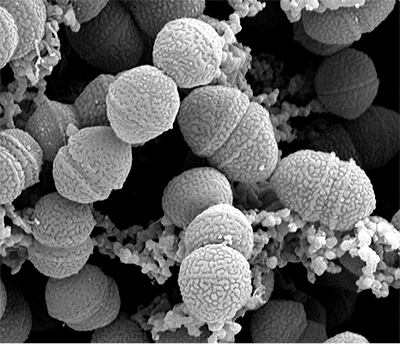
To test this hypothesis, we assembled an interdisciplinary team by bringing together faculty members associated with the Vanderbilt Pre-3 Initiative, a Trans-Institutional Program (TIPs) program that was launched in 2015. Our team consists of students from my organic chemistry lab, the Aronoff and Gaddy labs in the Division of Infectious Diseases and the Weitkamp team in the Department of Pediatrics. The program starts with the collection of human milk from patients at VUMC. From there, HMOs are isolated from the de-identified samples and analyzed using a variety of chemical techniques. Next, we complete microbiology studies in the Gaddy labs and work as a team to analyze the data. Thus far, we have validated the hypothesis in a seminal study published in the journal ACS Infectious Diseases, which revealed that HMOs from five women had the ability to inhibit the growth and biofilm production of Streptococcus agalactiae (Group B Streptococcus, GBS). In a follow-up study, we conducted a broader evaluation of the antimicrobial and antibiofilm activity by screening HMOs from 14 additional donors against three strains of GBS and two of the ESKAPE pathogens of particular interest to child health, Staphylococcus aureus and Acinetobacter baumannii. These studies validated that HMOs possess antimicrobial and antibiofilm activity against all three strains of GBS. They also showed that HMOs have antibiofilm activity against methicillin-resistant S. aureus and antimicrobial activity against A. baumannii.
It appears as though HMOs are narrow-spectrum antibiotics against GBS as characterized by the outstanding antimicrobial and antibiofilm profiles we have observed. In terms of antibiotic development, narrow-spectrum antibiotics are advantageous over traditional broad-spectrum antibiotics due to their lower susceptibility to resistance development and decreased collateral damage to the host. To compliment these advantages, HMOs are themselves nontoxic at all concentrations. Given the growing need for narrow-spectrum antimicrobial agents and the growing potential of HMOs to serve as antibacterials, future efforts are focused on assaying HMOs against additional species of Streptococcus as well as both Gram-positive and Gram-negative pathogens to further elucidate how HMOs work.
I invite you to ask a question or leave a comment in the space provided below, and I encourage you to return to this blog page often for future updates on the Pre3 Initiative.
One Comment on “Human Milk as a Source of Narrow Spectrum Antimicrobial Agents”
Karen Shindhelm on January 30th, 2018 at 12:39 pm
I really only would like to say, thank you for such fabulous research! I thoroughly enjoy reading new medical research and developments which stems from my nursing educator background and love for people: and their health! Great work!!